by Naseem S. Miller, The Journalist’s Resource
March 1, 2022
As the COVID-19 pandemic enters its third year, researchers are learning more about the long-term effects of the infection and about a collection of symptoms and complications commonly called long COVID.
Shortness of breath, fatigue and “brain fog” are among the most common symptoms of long COVID. For some, these symptoms persist after getting infected with coronavirus. For others, new complications arise weeks or months later.
There are many unanswered questions, like how common long COVID is, who is more likely to get it and why. And there’s still no consensus in the medical community over the definition, diagnosis and treatment of long COVID.
“I think we’re still scratching the surface,” says Dr. Amesh Adalja, a senior scholar at the Johns Hopkins University Center for Health Security, whose research focuses on emerging infectious disease, pandemic preparedness and biosecurity.
Below we have addressed some of the key questions about long COVID and summarized several studies that journalists can use to bolster their reporting. Keep in mind that knowledge and research in this field is rapidly evolving, and we will update this piece periodically as new analyses comes to light.
What is long COVID?
There’s no universal definition for long COVID.
The CDC says long COVID is a wide range of new, returning or ongoing physical and mental health problems people can experience four or more weeks after first getting infected with SARS-CoV-2, the virus that causes COVID-19.
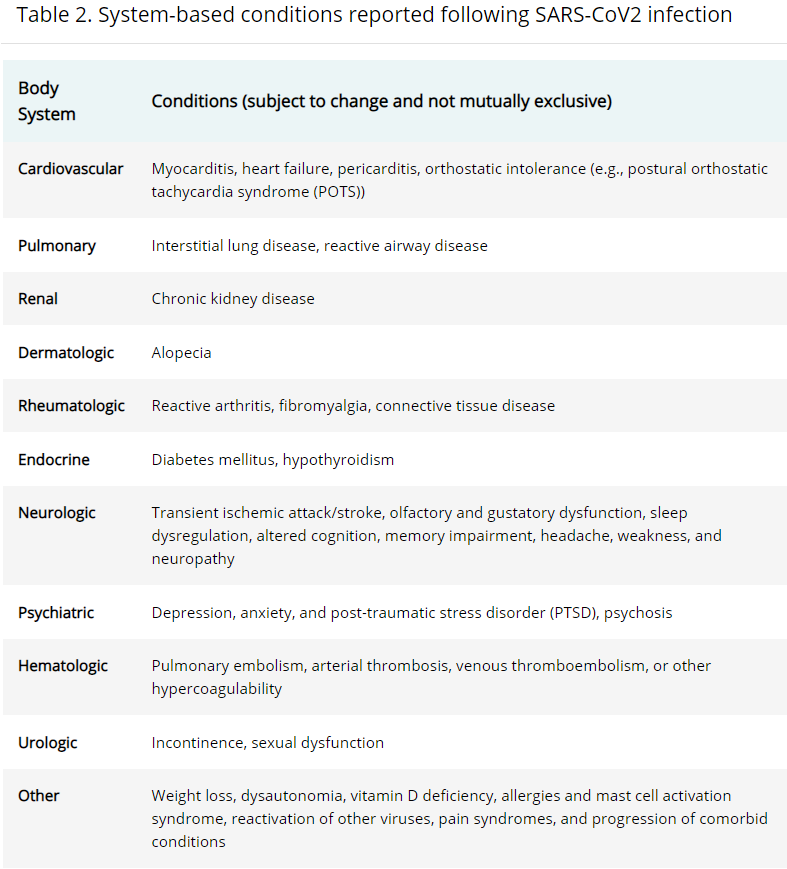
People with long COVID commonly have a combination of symptoms, including shortness of breath, fatigue, difficulty concentrating or thinking (“brain fog”), headache, sleep problems, dizziness, rash and joint or muscle pain, among others. Some people who develop a severe COVID-19 infection can also develop autoimmune conditions. Others may experience complications that affect their heart, lungs, kidneys or skin.
The World Health Organization has a wider window for symptoms that can be considered long COVID. Instead of the CDC’s four weeks, it says long COVID occurs “usually 3 months from the onset of COVID-19 with symptoms … that last for at least 2 months and cannot be explained by an alternative diagnosis.” These symptoms may have persisted since the initial illness, gone away and reappeared, or be new.
As of July 2021, long COVID can be considered a disability under the Americans with Disabilities Act, according to the U.S. Department of Health and Human Services.
Is “long COVID” the correct term?
The Centers for Disease Control and Prevention uses the umbrella term “post-COVID conditions.” It also lists other terms used for the condition, including long COVID, long-haul COVID, post-acute COVID-19, long-term COVID, chronic COVID, post-acute COVID syndrome.
Scientists use the umbrella term post-acute sequalae of SARS-CoV-2 infection, or PASC. Long COVID falls under this umbrella; so does multisystem inflammatory syndrome in children (MIS-C) and adults (MIS-A), which is a rare but severe immune response to COVID-19 infection.
The World Health Organization says, “Post COVID-19 condition, also known as ‘long COVID,’ refers collectively to the constellation of long-term symptoms that some people experience after they have had COVID-19. People who experience post COVID-19 condition sometimes refer to themselves as ‘long-haulers.’”
The Associated Press Stylebook recommends either “long-haul COVID-19” or “long COVID-19.” “We don’t use the medical term,” the stylebook says, referring to PASC. The New York Times uses “long Covid.”
What’s the difference between long COVID and Post-ICU Syndrome?
Patients who spend time in the ICU can develop post-intensive care syndrome, or PICS, which can include severe weakness, problems with thinking and judgement and post-traumatic stress disorder (PTSD), according to the CDC. PICS is a well-established medical diagnosis that existed long before COVID-19.
“It’s really important to separate long COVID from conditions such as post ICU syndrome, because anybody that’s admitted to the intensive care unit on a ventilator is not going to recover [quickly],” says Adalja.
Part of the current research is focused on distinguishing conditions that are only the result of COVID-19 infection from those that result from hospitalization and other treatments for severe illness from the infection.
“Some symptoms that can occur after hospitalization are similar to some of the symptoms that people with initially mild or no symptoms may experience many weeks after COVID-19,” according to the CDC. “It can be difficult to know whether they are caused by the effects of hospitalization, the long-term effects of the virus, or a combination of both.”
Who gets long COVID?
Long COVID can occur in people who get severely sick, have a mild illness or don’t have symptoms.
“Whereas older patients and those with underlying health conditions might have an increased risk for severe disease, young people, including those who were physically fit before SARS-CoV-2 infection, have also reported symptoms lasting several months after acute illness,” according to the CDC.
In September 2021, the National Institutes of Health announced the establishment of national study to “understand how people recover from COVID-19 and why some people do not fully recover after the viral infection seems to have cleared.” The study is called Researching COVID to Enhance Recovery Initiative, or the RECOVER Initiative. The project, which will include several universities and hospitals, is still in its initial phases and hasn’t enrolled patients yet.
How common is long COVID?
We don’t know yet, mainly because there’s a lack of long-term studies. Estimates of long COVID vary widely in the current literature, ranging from 5% to 80%, according to the CDC.
According to the World Health Organization, about 10% to 20% of people who get COVID-19 experience “mid- and long-term effects” after they recover from the initial illness.
According to the U.K.’s Office for National Statistics, an estimated 1.3 million people, or 2.1% of the population, self-reported long COVID. The estimate is based on a survey of 305,997 people over a four-week period ending on Jan. 2, 2022.
WHO has developed medical codes for long COVID, which can help with documentation and surveillance of the condition around the world.
Long COVID can also occur in children, but it appears to be less common than in adults. It has also been more commonly reported in women, but researchers don’t know why.
How is long COVID diagnosed?
Diagnosing long COVID isn’t simple. No laboratory test can definitively distinguish long COVID at this time. In its guidance to clinicians, the CDC recommends a list of tests for evaluating people for long COVID.
Some patients who develop long COVID may have never had a positive test for the infection or may have received a negative test because of waning antibody levels or false-negative results, the CDC explains.
Adalja says he first rules out post-ICU syndrome and other preexisting medical conditions that may have gone undiagnosed. He then looks to see if the patients’ lingering symptoms interfere with their daily activities. An example is someone who used to be able to go up the stairs but now gets winded after a few steps. He added that he doesn’t consider chronic cough to be a symptom of long COVID, because it occurs after many viral infections and can last weeks.
“And then you’re left in the end with a diagnosis of exclusion: No, they weren’t in the ICU. Yes, this [limits daily] activities. And no, this is not something that that’s caused by another illness that that could be present. And then you kind of back into the diagnosis of long COVID,” Adalja says.
The CDC notes that doctors shouldn’t solely rely on lab or imaging results to assess patients.
“Lack of laboratory or imaging abnormalities does not invalidate the existence, severity, or importance of a patient’s symptoms or conditions,” the agency says.
How is it treated?
There’s no single treatment or drug for long COVID, because it’s not just one illness. Many post-COVID conditions can improve through already-established approaches that manage symptoms, according to the CDC. For instance, breathing exercises can improve shortness of breath.
Across the U.S., hospitals and medical centers are establishing clinics for patients who have long COVID, bringing together different specialties to address the patients’ needs. At least 66 hospitals and health systems have post-COVID-19 clinics, according to Becker’s Hospital Review.
Many post-COVID conditions can also be managed by primary care providers, according to the CDC.
“It’s not going to be, in the end, something that is going to be amenable to ‘take this pill and your long COVID goes away,’” says Adalja. “And I think until we understand what’s going on in those patients, it’s more going to be like precision medicine than one size fits all.”
How can long COVID be prevented?
Do your best to not get COVID, says Adalja.
Research also suggests that vaccinated people are less likely to develop long COVID.
A briefing by the U.K. Health Security Agency, published on February 2022, examines 15 studies that reported on the effectiveness of vaccines against long COVID. It finds that people who are fully vaccinated against COVID-19 have a lower risk of developing long COVID compared with those people who are partially vaccinated or unvaccinated.
How does it compare with other infectious diseases?
COVID-19 is not the first infectious disease to have lingering effects.
After the 1918 flu, some people had long-haul flu symptoms called Von Economo Encephalitis, which the late, renowned physician and author Dr. Oliver Sacks later wrote about in his book “Awakenings,” turned into a namesake movie, says Adalja.
Other diseases that can have lingering effects include mononucleosis, or mono, and Lyme disease.
Who are the best sources for news stories about long COVID?
A range of medical specialties are involved in the care of patients who have long COVID, including infectious disease, critical care, cardiology, neurology, psychiatry, rheumatology, nephrology, pulmonology and physical medicine and rehabilitation.
Journalists Betsy Ladyzhets and Fiona Lowenstein have created a list of long COVID experts and advocates as a resource for other journalists. https://www.youtube.com/watch?v=5sjiXbvK-Ow Source: Harvard T.H. Chan School of Public Health
Below are summaries of several studies on long COVID.
Research Roundup
Prevalence of Select New Symptoms and Conditions Among Persons Aged Younger Than 20 Years and 20 Years or Older at 31 to 150 Days After Testing Positive or Negative for SARS-CoV-2
Dr. Alfonso Hernandez-Romieu; et al. JAMA Network Open, February 2022
The study aims to understand the prevalence of several symptoms among people who tested positive for COVID-19 compared with those who tested negative, between 31 and 150 days after initial COVID testing. It breaks down the findings by age and care setting. The study uses the National Patient-Centered Clinical Research Network, PCORnet, which has COVID-19 data from electronic health records of 42 health care systems. The study includes 338,024 people younger than 20 and 1,790,886 people 20 years and older. Among those, 168,701 people 20 years and older and 26,665 people younger than 20 tested positive for COVID-19. The individuals were tested for COVID-19 between March and December 2020 and had a doctor visit between 31 to 150 days after testing.
Findings: New diagnoses of shortness of breath were significantly higher among people with a positive COVID-19 test compared with those who tested negative for the virus, among all age groups.
Diagnoses of fatigue, cognitive dysfunction, sleep disorders, heart rate abnormalities, muscle and nerve disorders, and type 2 diabetes among hospitalized people 20 years or older, and heart rate abnormalities and type 2 diabetes among hospitalized people younger than 20 were more common for those with a positive COVID-19 test, compared with those who had a negative test.
The takeaway: “Although new symptoms and conditions occurred infrequently, applying the proportions of these rare events to the millions of persons infected with SARS-CoV-2 means that a substantial number might experience new symptoms and conditions after their acute illness,” the authors write. “In addition, new symptoms can be long-lasting and involve chronic conditions, such as type 2 diabetes.”
Health-care professionals should be aware of new symptoms and conditions that may develop after COVID-19 infection, particularly among hospitalized patients, the authors add.
Limitations: Researchers relied on diagnostic codes in electronic health records to identify symptoms. This could lead to underestimation of some conditions since coding practice may not be comprehensive during visits. Also, the code groups they used might have resulted in including symptoms and conditions unrelated to a COVID-19 infection, the authors note. In addition, they were unable to determine whether new symptoms and conditions were due to effects of the COVID-19 infection or the result of recognition of previously undiagnosed health problems. In addition, the team was unable to control for differences in demographic characteristics or underlying medical conditions.
Risks of Mental Health Outcomes in People with COVID-19: Cohort Study
Yan Xie, Evan Xu and Ziyad Al-Aly. BMJ, February 2022
The study aims to estimate the risk of developing mental health disorders among people who have had COVID-19. It uses data from the U.S. Veterans Health Administration, including 153,848 people who survived their first 30 days of COVID-19 infection and two control groups: one with no evidence of COVID-19 (5,637,840 people) and the other from before the pandemic (5,859,251 people).
Findings: People who had COVID-19 were 60% more likely to experience various mental health problems compared with the control groups. People with COVID-19 showed an increased risk of incident mental health disorders, including anxiety disorders, depressive disorders, stress and adjustment disorders, opioid use disorder, other (non-opioid) substance use disorders, neurocognitive decline, and sleep disorders, compared with the control groups, the authors write. The risks were highest in those who were admitted to the hospital during the initial phase of COVID-19 infection.
The takeaway: “The findings suggest that people who survive the acute phase of covid-19 are at increased risk of an array of incident mental health disorders,” the authors write. “Tackling mental health disorders among survivors of covid-19 should be a priority.”
Limitations: The demographic composition of the study is mostly older white men (76%), which might limit the generalizability of study results, the authors write. They study also didn’t examine the severity of the mental health outcomes. Also, it is possible that increased attention to people with COVID-19 might have resulted in greater diagnosis of mental health conditions compared with the control groups.
Another study by the team: “Long-term Cardiovascular Outcomes of COVID-19,” published in Nature Medicine in February 2022, shows that people with COVID-19 are at increased risk of developing heart conditions compared with control groups.
Short-term and Long-term Rates of Postacute Sequelae of SARS-CoV-2 Infection. A Systematic Review
Destin Groff; et al. JAMA Network Open, October 2021
The systematic review includes 57 studies from 16 countries, including the U.S., published between December 2019 through March 2021, with a total of 250,351 COVID-19 patients, 79% of whom were hospitalized during initial infection.
Findings: More than half of the patients had long COVID six months after recovering from the initial infection. The most common symptoms were abnormalities in chest imaging, difficulty concentrating, anxiety and fatigue or muscle weakness. “Other frequently reported symptoms included cardiac, dermatologic, digestive, and ear, nose, and throat disorders,” researchers write.
The reasons for complications after COVID-19 infection are not understood, the authors note.
“Nevertheless, these mechanisms can be grouped into the direct effect of the viral infection and the indirect effect on mental health due to posttraumatic stress, social isolation, and economic factors, such as loss of employment,” they write.
What’s missing: “No clear guidelines are currently available” on how to care for patients after an initial COVID-19 infection, the authors note. “And there is a notable dearth of information on and strategies about how to assess and manage patients following their acute COVID-19 episode,” they write. Part of the reason, they add, is because there’s no universal definition of long COVID.
Recommendations: The authors write that the clinical management of long COVID will require a “whole-patient perspective.” They recommend one-stop multidisciplinary clinics “to avoid multiple referrals to different specialists and encourage comprehensive care,” they write. “These specialists should include respiratory physicians, cardiologists, neurologists, general physicians (from primary care or rehabilitation medicine), neuropsychologists or neuropsychiatrists, physiotherapists, occupational therapists, speech and language therapists, and dieticians.”
The bigger picture: Long COVID can overwhelm the capacity of current health care systems, particularly in low- and middle-income countries.
Limitations: Researchers point out there’s no consensus on the definition of long COVID, which makes comparison of studies and their patient populations difficult. Also, researchers couldn’t separate out the risk of long COVID based on the severity of initial illness, by existing underlying medical conditions, or by age. They also note that most studies only looked at specific symptoms and didn’t report all the symptoms that patients experienced at various points.
Multiple Early Factors Anticipate Post-Acute COVID-19 Sequelae
Yapeng Su; et al. Cell, January 2022
The study: Researchers followed 209 COVID-19 patients for two to three months after an initial diagnosis in 2020 and early 2021. Using blood samples, they looked for biological factors that could be associated with the risk of developing long COVID. The patients were from five Swedish Medical Center hospitals and clinics in the Puget Sound region near Seattle. Their average age was 56, ranging from 18 to 89 years. The study also had 457 healthy adults as the control group.
Findings: The team identified four factors that could be associated with higher risk of developing long COVID: existing type 2 diabetes; reactivation of Epstein-Barr virus, a common virus that can cause mono and usually turns dormant after infection; presence of autoantibodies, which can attack normal cells by mistake and are one of the hallmarks of autoimmune diseases such a psoriasis and rheumatic arthritis; and a high level of coronavirus RNA in the blood.
Limitations: The authors note that their study follows patients only 2 to 3 months after an initial infection and can’t predict which patients will have chronic symptoms of long COVID. They also add that the study size was not large enough to establish specific predictors of long COVID.
Characterizing Long COVID in an International Cohort: 7 Months of Symptoms and Their Impact
Hannah Davis; et al. EClinicalMedicine, July 2021
The study aims to better understand the range of symptoms in patients with long COVID, their daily function and return to pre-COVID health. It is based on the results of an online survey of 3,762 participants with confirmed or suspected COVID-19 from 56 countries, including the U.S. The survey was distributed on long COVID support groups and social media between September and November 2020. Most respondents were women (78.9%) and white (85.3%). Most were also between 30 to 59 years old. The participants were followed for seven months.
Findings: The most frequent symptoms six months after the initial infection were fatigue, worsening of symptoms after minor physical or mental activity (post-exertional malaise) and cognitive problems. For more than 91% of respondents, recovery from symptoms took more than 35 weeks. More than 88%, across age groups, reported memory and cognitive problems. About 45% needed a lighter work schedule after COVID-19 infection and 22.3% said they weren’t working at the time of the survey because of their illness. Other symptoms participants mentioned included new allergies, seizures, suicidality, changes in sensitivity to medication, vision loss, hearing loss and facial paralysis, the authors note.
The takeaway: “Overall, these findings suggest that the morbidity of COVID-19 illness has been greatly overlooked,” the authors write. “Patients experience multisystem symptoms for over seven months, resulting in significant impact to their lives and livelihoods.”
Limitations: The study is based on a survey, so how the participants recalled their experience could have impacted the estimates, according to the authors. Also, overreporting and underreporting of symptoms are possible, the authors note. Another limitation is sampling bias toward long COVID patients, since the survey was distributed in long COVID online support groups. The survey also required participants to have stable internet and email addresses, potentially excluding some groups, including low-income individuals.
Additional resources
- CDC’s main page for long COVID.
- CDC’s interim guidance on evaluating and caring for patients with post-COVID conditions.
- CDC’s list of long COVID support groups.
- Video from the National Institutes of Health: Understanding Long COVID Across Communities of Color and Those Hardest Hit by COVID, February 2021.
- Coronavirus Disease (COVID-19): Post COVID-19 Condition. A Q&A from the World Health Organization, December 2021.
- In the Wake of the Pandemic, Preparing for Long COVID, Policy Brief 39, World Health Organization, February 2021.
- What is Long Haul COVID? A presentation by the Mayo Clinic’s Dr. Greg Vanichkachorn for Minnesota House’s Health Finance and Policy Committee, February 2022. You can find the audio of the presentation here.
- “Post-Acute COVID-19 Syndrome and the Cardiovascular System: What Is Known?” Neal Dixit; et al. American Heart Journal Plus: Cardiology Research and Practice, June 2021.
- “6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records” Maxime Taquet. Lancet Psychiatry, May 2021.
Suggested reading
- “One journalist’s journey to uncovering the truth behind long-COVID treatments,” by Bara Vaida and Paula Rodriguez, The Association of Health Care Journalists, February 2022.
- “What is long covid? Current understanding about risks, symptoms and recovery.” by Allyson Chiu, The Washington Post, February 2022.
- “‘I had never felt worse’: Long Covid sufferers are struggling with exercise,” by Melinda Wenner Moyer, The New York Times, February 2022.
- “How long Covid exhausts the body,” by Josh Keller, The New York Times, February 2022.
- “Long-haul COVID cases could spike after latest wave,” by Melinda Wenner Moyer, Scientific American, February 2022.
- “Controlled studies ease worries of widespread long Covid in kids,” by Shelli Farhadian and Shira Doron, STAT, February 2022.
- “What doctors wish patients knew about long COVID,” by Sara Berg, American Medical Association, October 2021.
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.![]()